Oxalates: Their Influence on Chronic Disease
New science and clinical experience reveal concerns about oxalates that far exceed traditional kidney stone pathology. In order to best support their patients and clients, integrative practitioners, and especially diet and nutrition specialists would benefit from greater understanding of their influence.
Oxalates are highly reactive molecules; they present in our body as sharp crystals or crystalline structures with jagged edges that cause pain, irritation, and distress. They can bind with certain minerals; particularly calcium and magnesium, as well as iron and copper.
Having high oxalate in the body can be problematic; and not giving proper consideration to one’s oxalate intake can impede the effectiveness of even the best healing diet protocol.
High oxalate in the body (hyperoxaluria) can be a factor in many chronic conditions; including digestive issues, autoimmune disorders, and neurological conditions. Oxalates affect mitochondrial function and can create inflammation; thus influencing every system in the body.
This article explores the repercussions of the oxalate cascade in a variety of chronic diseases; and my follow-up article will specifically investigate oxalates and autism – and how you, the knowledgeable practitioner, can help.
Understanding Oxalates
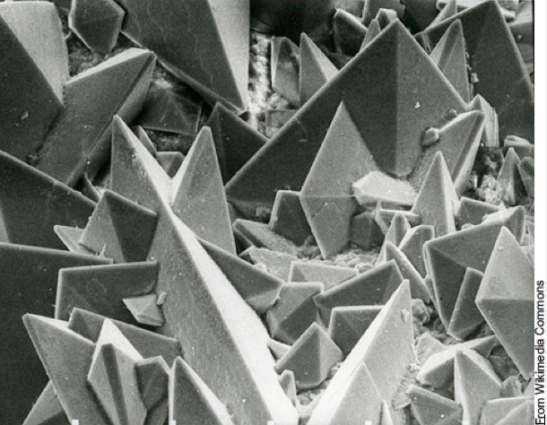
Although most commonly identified with the formation of calcium oxalate kidney stones (oxalate bound to calcium), when unbound, free oxalate can interfere with cellular functions; affecting health on a broader, systemic level.
Clinical studies and anecdotal experience indicate that oxidative stress, mitochondrial disruption and damage, and nutrient depletions, trigger widely varied symptoms including fatigue and inflammatory cascades, joint pain or pain anywhere in the body.
Chronic low energy is very common because of a reduction in ATP in the mitochondria. Oxalates could be a hidden source of headaches, urinary pain, genital irritation, joint, muscle, intestinal or eye pain.
Other common oxalate-caused symptoms may include mood conditions, anxiety, sleep problems, weakness, or burning feet. Indicators can be digestive, respiratory, or even bedwetting for children.
It’s important to note that oxalates can inhibit the absorption of calcium, magnesium, and other minerals; which actually makes oxalates an “anti-nutrient.” Minerals in food become bound by oxalate – for instance calcium (thereby forming insoluble calcium oxalate) – and cannot then be absorbed properly by the intestinal tract. This can lead to mineral deficiencies, such as calcium and/or magnesium deficiency.
In the gut of a healthy person, oxalates typically bind together with these minerals (are not absorbed through the gut), then eliminated in the stool. While this inhibits absorption of nutrients, beneficially this ensures they are excreted rather than crossing the gut into the blood stream and causing cellular distress and damage.
High Oxalate
Once oxalate gets into cells where it can disrupt mitochondrial function; it can cause all sorts of systemic disturbances. Here are some of the varied effects of high oxalate in the cells and tissues – that we’ll explore through the course of this article:
- Disrupt mineral absorption and usage
- Impair cellular energy
- Deplete nutrients like glutathione and interfering with biotin
- Create oxidative stress[1]
- Activate the immune system to trigger inflammatory cascades
- Interfere with and damage mitochondrial function[2]
- Damage cells and tissues
- Cause seizures during toxic exposure to oxalate[3],[4],[5]
- Cause faulty sulfation
- Cause histamine release
Types & Sources of Oxalates
Oxalates stem from two main sources: exogenous (outside the body; from dietary intake) and endogenous (produced within the body, cell or tissue).
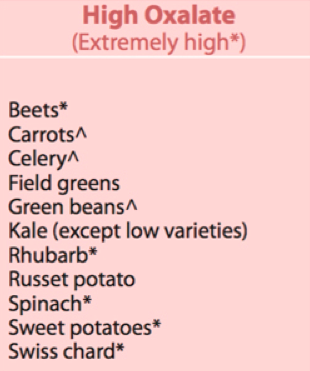
Exogenous oxalate can accumulate from a diet that is high in spinach, nuts, beans, or other high oxalate foods. This is why individualizing therapeutic diets is essential; because “by the book” some well-known special diets strongly rely on higher-oxalate foods (especially almonds/almond flour).
Diets often heavy on these nut flours include: SCD, GAPS, and Paleo. And vegetarian diets are often high in oxalate; since they usually include many beans, grains, nuts and seeds, as well as high oxalate greens or starchy vegetables, like spinach or sweet potatoes.
Practitioners should be aware that diets high in oxalate could create a wide variety of problems for some people. Making informed choices or modifying a diet for oxalate can make a dramatic difference in lowering the oxalate load (note: it is important to reduce oxalates in the diet very slowly).
However, most of our body’s total oxalate content is created during normal body metabolism. “It is increasingly accepted that 80-90% of urinary oxalate is produced endogenously,” [6] within the cell, and this can directly wreak havoc in the body.
Read the rest of this article that includes information on:
The Origin of Oxalate Issues
- Deficiencies and Endogenous Production
- When the Gut is Unhealthy
- Sulfate, Poor Sulfation, and Mitochondrial Dysfunction
Effects of High Oxalate in the Body
- Mitochondrial Dysfunction
- Oxidative Stress, Inflammation, and Glutathione
Read the original full text article at: http://bioindividualnutrition.com/oxalates-their-influence-on-chronic-disease/