How Environmental Toxins and Glyphosate Damage the Thyroid
A vast amount of research shows that glyphosate pesticides and other toxins, which are ubiquitous in our environment, impact our fragile but powerful thyroid gland and can increase the risk of hypothyroidism, even beginning in the womb.
Because so many pesticides work on the nervous system, scientists are increasingly discovering the pesticide-related hypothyroidism risks come in part from the impact on the brain’s communication with the thyroid.
What you’ll learn:
- One of the primary ways pesticides appear to impact thyroid function is by disrupting communication between the brain, the pituitary gland, and the thyroid gland. This is called the hypothalamus-pituitary-thyroid (HPT) axis.
- Although organochlorine pesticides (OCPs) like DDT have been banned, they still persist in the environment and impact thyroid health, especially in pregnant women and children. They can also worsen the impact of pesticides currently in use.
- Glyphosate is most commonly associated with the pesticide Roundup weed killer and is linked with an increased risk of hypothyroidism.
- Carbamates are widely used in agriculture as insecticides, herbicides, and fungicides and have been linked to lower thyroid function through their impacts on thyroid enzymes.
- Pyrethroids are synthetic versions of the natural pest deterrent pyrethrin and are abundant in the environment due to their wide use globally. One of their mechanisms is to compete with thyroid hormones at the receptor site.
- Phenylpyrazole is primarily found in the product ingredient fipronil, which is widely used in urban and veterinary applications for pest control. It inhibits thyroid function.
- Neonicotinoids are insecticides that were discovered in the 1980s and are widely used in agricultural, commercial, residential, and veterinary settings. They have been shown to disrupt thyroid function and decrease thyroid hormones, not to mention contribute to the collapse of the bee population.
Synthetic pesticides started to become widely used in the 1940s, and although they significantly increased crop yields (1) (2) (3), they also showed alarming effects on health. While those warnings were ignored over the years as the number of pesticides introduced to the market grew, scientists continued to study (4) their effects on human health.
One trend that has consistently emerged is the link between pesticides and their impact on thyroid health and function, contributing to symptoms of hypothyroidism (low thyroid function) and other thyroid disorders.
The warning bells first rang in the early 1960s when researchers discovered pesticides thinned the eggshells of wild birds due to impact on the endocrine, or hormonal, system (5) (6). Since then, researchers have been studying the impacts of pesticides on human health (7) (8).
The term “endocrine disrupter” was coined in the early 1990s to describe the way pesticides interfere with (9) (10):
- Thyroid hormones
- Estrogens
- Male hormones like testosterone
- Adrenal hormones like cortisol
While the effects of acute exposures on workers in the pesticide industry have been well researched (11) (12) (13), the impact of lower level but cumulative contamination from everyday exposure is less studied (14). Pesticides are abundant not only in agriculture, but also in urban and suburban environments, schools, lawns, playing fields and golf courses, and perhaps even in your own garden.
Given that even low levels of exposure of many pesticides have been shown to disrupt the endocrine system (15) (16) (17) (18), understanding the risks to your thyroid health is vital. This is especially true during pregnancy and early motherhood when the developing fetus and infant are more vulnerable (19) (20).
How Pesticides Affect Communication Between the Brain and the Thyroid
Every cell in the body uses thyroid hormone, so thyroid activity is necessary for every organ and system. However, the thyroid gland is best known for its role in regulating metabolism, which is why thyroid disorders often manifest as weight gain, weight loss resistance, and feeling cold all the time (21) (22).
In children, healthy thyroid function ensures proper brain development (23); thyroid dysfunction during early pregnancy can impact the child’s IQ later in life (24) (25) (26).
In fact, a 2015 European study estimated the impacts of endocrine disrupting pesticides on childhood brain development disorders costs more than 150 billion Euros, or $162 billion annually due to low IQ, autism spectrum disorders, attention deficit/hyperactivity disorder (ADHD), and other issues in children (27).
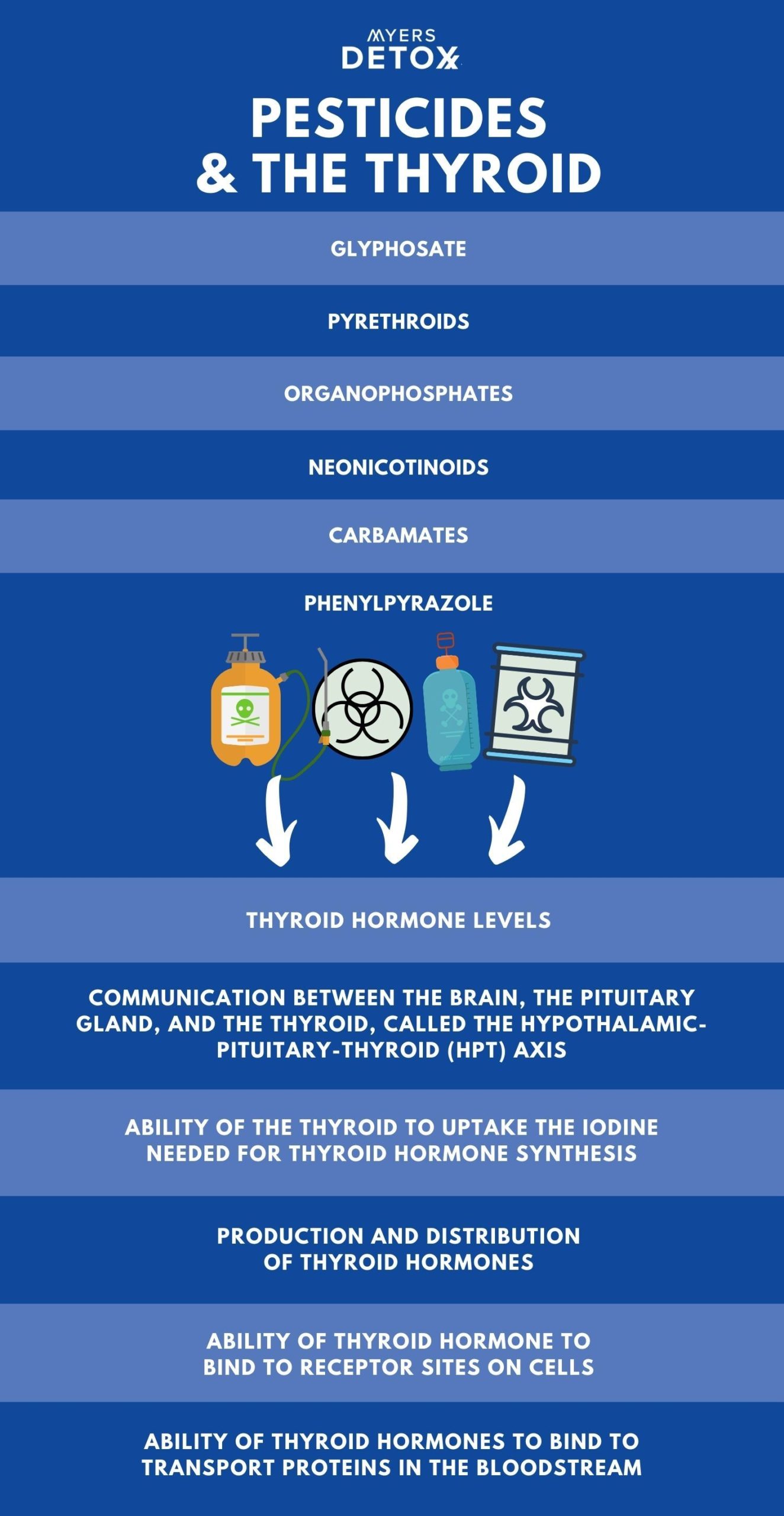
Studies show pesticides impact the following areas of thyroid function (28) (29) (30) (31) (32) (33):
- Thyroid hormone levels
- Communication between the brain, the pituitary gland, and the thyroid, called the hypothalamic-pituitary-thyroid (HPT) axis
- Ability of the thyroid to uptake the iodine needed for thyroid hormone synthesis
- Production and distribution of thyroid hormones
- Ability of thyroid hormone to bind to receptor sites on cells
- Ability of thyroid hormones to bind to transport proteins in the bloodstream
Following is a more detailed breakdown of how different classes of pesticides like glyphosate affect thyroid function.
How Organochlorine Pesticides (OCPs) Damage the Thyroid
Studies on the effects of organochlorine pesticides (OCPs) like DDT on mothers and their children have found associations with either an increase in thyroid-stimulating hormone (TSH), which regulates thyroid activity, a decrease in circulating thyroid hormones throughout the body, or both.
Even though most OCPs have been banned, they persist in the environment and in human tissues, and may exacerbate or potentiate the harmful effects of newer pesticides commonly used today.
OCPs were the first generation of synthetic pesticides and were used extensively globally until the 1960s. They include DDT and the fungicide hexachlorobenzene. OCPs work by disrupting the nervous systems in insects (34).
Effective and cheap, DDT was once widely used around the world (35) until its harmful effects on wildlife were discovered (36). Public outcry over DDT eventually played a role in the creation of the Environmental Protection Agency and the ban of many OCPs in the 1970s.
Despite the ban, OCPs are still very prevalent in the environment and continue to impact human and animal health. Because they do not easily break down, they accumulate in body tissue, persist in the soil and are still found throughout the food chain (37) (38).
OCPs are associated with poor brain development in infants and children (39) (40) (41) (42) (43) (43) (44) (45) (46) (47) (48), which is believed to stem from the impact of OCPs on the hypothalamic-pituitary-thyroid axis (HPT) between the brain and the thyroid in pregnant women and newborns. (49) (50) (51) (52) (53) (54) (55) (56) (57) (58) (59) (60)
The HPT axis is a delicate feedback loop that signals to the glands how much thyroid hormone to produce. The hypothalamus is the area of the brain that governs hormone function. The pituitary gland, located at the base of the brain, secretes hormones that regulate the body’s other hormone glands.
A number of studies on pregnant mothers and children have shown OCPs lower thyroid hormones and thyroid hormone activity in both mothers and newborns. The studies also showed OCPs elevate thyroid-stimulating hormone (TSH).
High TSH is a primary marker for a hypothyroidism diagnosis (low thyroid). When the thyroid is under functioning, TSH goes up in an attempt to tell the brain to raise thyroid hormone levels.
One interesting exception was among a fishing population in Canada (61) that did not show similar impacts. The study’s authors considered the higher intake of dietary iodine and selenium may have buffered the thyroid from the damaging effects of OCPs.
Most people are deficient in iodine and selenium. I always recommend clients to take these two minerals as they are so important for proper thyroid functioning.
Gender also affects outcomes. A 2015 study of the French Caribbean where OCPs were used until 1993 showed that prenatal exposure to OCPs raised TSH in boys (remember, higher TSH means lower thyroid function).
However, in female infants, postnatal exposure was associated with lower thyroxine (T4), the primary thyroid hormone secreted by the thyroid gland, and lower triiodothyronine T3 in both girls and boys (62). T3 is the active form of thyroid hormone that the body’s cells can use.
Studies on the impacts of OCPs on adults are less straightforward. Some show they are linked to higher rates of hyperthyroidism (like in Grave’s disease, an autoimmune disease that causes the thyroid to be overactive) in men (61), aging women (62), and occupational workers (63).
Other studies show OCPs related to hypothyroidism in women (64), elderly men (65), adolescents (66) and pesticide workers that apply pesticides (67) (68) (69) (70) (71).
How are OCPs inhibiting thyroid function specifically? Animal studies suggest that OCPs:
- Impact the proteins that transport thyroid hormones in the blood,
- Increase the clearance of thyroid hormone in the liver,
- Impact receptor sites for thyroid hormone in the brain, and
- Mimic thyroid hormones and competing with them at cellular receptor sites (72) (73) (74) (75) (76) (77).
Long term exposure to low levels of DDT has been shown to change the structure of thyroid tissue to compensate for lowered thyroid hormone activity (78) (79).
In vitro (test tube or petri dish) studies suggest DDT alters cell membranes to cause receptors for TSH to fail (80) (81) (82), negatively impact thyroid hormone production (83), and dysregulate thyroid specific gene function (84).
In summary, studies on OCPs have identified numerous ways in which they inhibit thyroid function and cause symptoms of hypothyroidism or hyperthyroidism.
How Organophosphate Pesticides Disrupt Thyroid Function
Organophosphate pesticides (OPPs) are another type of pesticide, the first application having been as nerve gas in World War II. Because OPPs work similarly on the insect nervous system as they do on the human’s, they were soon introduced for agricultural use (85).
This is unfortunate because studies soon showed that even low levels affected fetal brain development (86) (87). Although most developed countries have phased out use of OPPs, their agricultural use continues to grow in developing nations worldwide (88).
Organophosphates have been associated with thyroid dysfunction (89), increase of hypothyroidism (90) (91) (92), brain function impairment (93) (94), and an increase in hormone-dependent cancers (95).
Research shows that urinary prenatal levels of OPPs are associated with reduced intellect (96), differences in brain structure (97), and higher TSH levels in children, thus indicating compromise of thyroid function (98).
In adults, exposure to OPPs has been shown to raise the risk of developing breast, thyroid, and ovarian cancers, and lymphoma (99). A study on pregnant women showed urinary levels of OPPs were associated with a negative impact on thyroid function (100).
Animal studies using environmentally relevant (not exaggerated) amounts of OPPs also show evidence of thyroid damage. Pre- and post-natal exposure resulted in maternal hypothyroidism and long-term reduction in the thyroid hormone T4 in offspring (101) (102).
Researchers also noted that manufacturers do not disclose the link between OPPs on poor cerebellum development, which they hypothesized stems from thyroid hormone deficiency in the developing fetus (103).
Fish studies have found OPPs interfere with maturation by disrupting thyroid function, altering genes, and lowering thyroid hormone levels, (104) (105) (106) (107), thus affecting the survival of fish in areas contaminated by OPPs (108).
How Glyphosate Damages the Thyroid
Glyphosate is an organophosphate compound used globally to kill weeds, its use having increased significantly since the mid 1990s not only on crops, but on city parks and playgrounds and on residential yards.
Glyphosate is the most used agriculture chemical ever. The most commonly known glyphosate is Roundup weed killer(109).
Trends in glyphosate herbicide use in the United States and globally, reveals that since 1974, when Roundup was first commercially sold, more than 3.5 billion pounds (or 1.6 billion kilograms) of glyphosate has been used in the U.S.. Compare that to the 18.9 billion pounds (or 8.6 billion kilograms) of glyphosate that has been used around the globe. It’s shocking to think the toll this has taken on human and animal health.
One study of more than 35,000 licensed pesticide applicators in the U.S. showed glyphosate was associated with increased risk of hypothyroidism (110), although these results conflict with other research (111) (112).
However, a rat study of pregnant rats exposed to glyphosate showed their thyroid-related genes behaved differently compared to control rats. They showed lower TSH levels (113), which could result from the changes in gene expression and alterations in the HPT axis. When function of the pituitary, the master hormone gland, is suppressed, this can result in low TSH (114) (115).
Researchers state that more studies are needed on the effects of glyphosate on the thyroid as well as on the gut microbiome, which could also impact genetic and thyroid function.
How Carbamates Reduce Thyroid Function
Carbamates work similarly to organophosphates on the nervous system and are widely used in agriculture as insecticides, herbicides, and fungicides (116). They have been shown to inhibit the thyroid peroxidase (TPO), an enzyme necessary to produce thyroid hormones (117) (118) (119).
While exposure is primarily of concern to farm and industrial workers, carbamates also make their way into the food supply of the average consumer (120). For instance, studies in Taiwan and Italy showed subjects with elevated levels of carbamates and OPPs had a significantly higher risk of developing hypothyroidism than the general population (121) (122).
Rat research has shown that carbamates impact thyroid-releasing hormone and thyroid enzyme activity, thus promoting hypothyroidism (123) (124) (125).
Hamster studies show carbamates impact thyroid development (126), while a study of zebrafish embryos exposed to carbamates showed altered thyroid genes and delayed hatching, increased mortality, and produced skeletal defects (127).
How Pyrethroids Alter Thyroid Hormone Levels
While pyrethrins, which are found in Chrysanthemum flowers, naturally protect against insects (128), they are not used commercially much as they break down quickly. Therefore, manufacturers created a synthetic version called pyrethroids, which act on the nervous system of insects (129).
Pyrethroids are used widely around the world (130), and most people are exposed through foods contaminated with the compound (131). They are found in soil, food, environmental, and human samples (132) (133) (134) (135) (136), most likely due to their excessive use.
Pyrethroids structurally resemble the thyroid hormones T3 and T4, which means they compete with thyroid hormone at cellular receptor sites, thus causing symptoms of deficiency (137).
Human exposure is widespread (138), and prenatal exposure via the placenta can impair normal development by impacting thyroid receptor site function, although more research is needed in this area (139) (140) (141).
Rat studies of pyrethroid exposure shows it alters levels of thyroid hormone (142) (143), impacts thyroid genes in the placenta of pregnant rats, and inhibits growth of the fetus (144).
Both lizard and fish studies showed pyrethroids alter thyroid-related genes (145) (146) and disrupt communication between the pituitary gland and the thyroid via the HPT axis (147).
Another fish study showed they impact the signaling behavior of thyroid hormones and thus development of embryos (148) (149).
How Phenylpyrazole Inhibit Thyroid Hormones
Phenylpyrazole is primarily found in the product ingredient fipronil, which is widely used to kill termites, ants, and roaches. Pets and humans are exposed via flea and tick collars and flea prevention medications like Frontline, Sentry Fiproguard, PetArmor, and Hartz First Defense. (150).
Fipronil’s popularity (151) (152), has led it to become a widespread environmental contaminant found in both soil, water (153) (154), dust (155), and foods (156) (157).
Most European nations restricted fipronil in 2013 after it was found to play a large role in the mass deaths of honeybees (158), although this ban has since been overturned (159).
Unfortunately, while it kills pests, it also kills beneficial insects and adversely affects fish, reptiles, birds, and mammals (160) (161) (162) (163) (164) (165) (166) (167) (168) (169).
In studies of factory workers who manufacture veterinary drugs, fipronil exposure is associated with inhibited secretion of TSH (170). Studies on the general population show fipronil transfers to the fetus through the placenta and is correlated with lower levels of T3 in newborns (171) and poor Apgar scores, a method used to assess newborns after birth (172).
In rat studies, fipronil exposure caused tumors via excess growth of thyroid follicles (173), disrupted the development of thyroid tissue (174) (175), and decreased levels of circulating thyroid hormone levels (176) (177) (178) (179).
How Neonicotinoids Decrease Thyroid Function
Neonicotinoids are insecticides that were discovered in the 1980s and are widely used in agriculture (180), and commercial, residential, and veterinary settings (181). In fact, only glyphosates are more popular (182) (183). Neonicotinoids are banned in Europe for killing bees and other pollinators.
As the name suggests, they are structurally similar to nicotine, which was once used as an insecticide, and disrupts the nervous system of insects (184) (185).
One study shows a connection between prenatal exposure to neonicotinoids and reduced IQ (186).
Other research shows exposure disrupts thyroid function in male finches (187), with excessive growth of the thyroid gland, and decreases in thyroid hormones.
How the Interaction of Pesticides Worsen Thyroid Function
Although scientists have studied some of the tens of thousands of chemicals in our environment, it’s important to consider how toxins affect our health when combined, as pesticides often are for agricultural use (188).
Chemicals can interfere or interact with one another (189), and health impacts can manifest when chemicals are combined that were not found when they were studied in isolation (190) (191) (192). These chemicals can potentiate each other, making them more toxic than when exposed to a single chemical.
For instance, animal studies show combining pesticides worsens the impact on thyroid hormone synthesis (193), thyroid genes (194), weight gain due to lowered thyroid hormone activity (195), thyroid gland function (196), and thyroid development (197) (198). In some cases, these effects were observed when exposure was at lower levels than what currently exists in the environment.
Unfortunately, however, few studies exist examining the effects of pesticides in combination and researchers are calling for more studies.
A Need for Improved Safety Testing of Pesticides
Clearly, we need more research and more acceptance of approaches to improve safety and better ensure thyroid health (205). This would not only better protect our health and that of our children, but also that of our pets, wildlife, and the environment (206).
In 2018, the European Union adopted criteria for identifying harmful pesticides (207) and the risks of pesticide mixtures to thyroid health are increasingly being recognized (208), but major safety gaps still exist throughout the world.
While TSH, T3, and T4 are the most common markers to measure the impact of pesticides on the thyroid, we also need to include evaluating the impact on the HPT axis given most pesticides work on the nervous system.
Although all classes of pesticides are associated with disrupting the delicate HPT axis, manufacturers are not required to research this potential action before releasing a new compound to the market.
The Takeaway When it Comes to Pesticides and Hypothyroidism
Hypothyroidism affects more than 20 million Americans, or about 12 percent of the population. Hashimoto’s is one of the most common autoimmune diseases today, affecting millions more. Given this, it should come as no surprise that thyroid hormone is one of the number one medications prescribed.
Additionally, we have been seeing a staggering rise in neurodevelopmental disorders in children and neurodegenerative disease in adults, which has drawn attention to the widespread use of pesticides in our environment (199).
Healthy brain function is required for healthy thyroid function, and numerous studies show how pesticides like glyphosate negatively impact communication between the brain and the thyroid (200) (201).
Also, it’s important to remember that the impact of pesticides on health are not going to cause immediate symptoms but instead do their work cumulatively over time. Consistent exposure to pesticides can change how the immune system functions, which may make a person more vulnerable to developing an autoimmune disease such as Hashimoto’s hypothyroidism.
What I have noticed over the years working with clients is that many times their symptoms are not resolved simply by taking thyroid medication. Many do see improvement, but others need to increase the dosage over time when the previous dose is no longer working. Still others increase the dosage and still do not see mitigation of their symptoms. I believe these pesticides interfere in thyroid hormone effectiveness and uptake at receptor sites just like they interfere in our body’s own hormones. .
Given these potential issues, it’s important to practice a detox lifestyle, reducing exposures in food and avoiding use of pesticides around the home and with pets. Most importantly, I advise adopting a detox program or protocols (like infrared saunas) that reduce the toxic load of these pesticides and chemicals in the body and fat tissues.
How to Detox and Protect Your Thyroid From Pesticides
Pesticides are ubiquitous in our environment and we need to use safe and natural tools daily to keep the thyroid detoxed and healthy.
Even though your goal may be to protect your thyroid, you need to think in terms of systemically detoxing pesticides and other environmental toxins like heavy metals from your entire body.
The goal to detox the thyroid and protect it daily from pesticides and toxins is a multi-step process:
- Taking substances like chelators that mobilize pesticides, heavy metals and toxins from body tissues like the fat, tissues, organs and glands.
- Bind the toxins that have been mobilized by supplements or infrared saunas so they don’t lodge elsewhere in the body
- Support the body’s pathways of elimination so they can exit the body (like supporting liver and lymph function).
- Mineralize the body so heavy metals and toxins don’t take the place of valuable minerals due to deficiency.
- Employ detox protocols like infrared saunas to hasten detox of body tissues and glands like the thyroid.
If you’d like to learn more about detoxing our body systemically, which will promote better thyroid hormone production, please inquire about our various other programs to detox the body of toxins like pesticides and heavy metals.
Click Here for References+
- Carvalho FP. Pesticides, environment, and food safety. Food Energy Secur. (2017) 6:48–60. doi: 10.1002/fes3.108
- Zhang W, Jiang F, Ou J. Global pesticide consumption and pollution: with China as a focus. Proc Int Acad Ecol Environ Sci. (2011) 1:125–44.
- Food and Agriculture Organization of the United Nations (FAO). FAOSTAT. (2019).
- Leemans M, Couderq S, Demeneix B and Fini J-B (2019) Pesticides With Potential Thyroid Hormone-Disrupting Effects: A Review of Recent Data. Front. Endocrinol. 10:743. doi: 10.3389/fendo.2019.00743.
- Peakall DB, Lincer JL, Risebrough RW, Pritchard JB, Kinter WB. DDE-induced egg-shell thinning: Structural and physiological effects in three species. Comp Gen Pharmacol. (1973) 4:305–13. doi: 10.1016/0010-4035(73)90013-X
- Ratcliffe DA. Changes attributable to pesticides in egg breakage frequency and eggshell thickness in some British birds. J Appl Ecol. (1970) 3:147–68. doi: 10.2307/2401998
- Yusa V, Millet M, Coscolla C, Roca M. Analytical methods for human biomonitoring of pesticides. A review. Anal Chim Acta. (2015) 891:15–31. doi: 10.1016/j.aca.2015.05.032
- Köhler H, Triebskorn R. Wildlife ecotoxicology of pesticides: can we track effects to the population level and beyond? Science. (2013) 341:759–66. doi: 10.1126/science.1237591.
- Colborn T, Clement C. Chemically-Induced Alterations in Sexual and Functional Development: The Wildlife/Human Connection, Volume 21, Advances in Modern Environmental Toxicology. Princeton, NJ: Princeton Scientific Publishing Co., Inc. (1992).
- Colborn T, Dumanoski D, Myers JP. Our Stolen Future?: Are We Threatening Our Fertility, Intelligence, and Survival? A Scientific Detective Story. (1996). European Commission. EU Pesticides Database – Fipronil.
- Alewu B, Nosiri C. Pesticides and human health. In: Pesticides in the Modern World – Effects of Pesticides Exposure. InTech. p. 303–14.
- Lushchak VI, Matviishyn TM, Husak VV, Storey JM, Storey KB. Pesticide toxicity: a mechanistic approach. Excli J. (2018) 17:1101–36. doi: 10.17179/excli2018-1710
- Hutter H, Moshammer H. Pesticides are an occupational and public health issue. Int J Environ Res Public Health. (2018) 15:1650. doi: 10.3390/ijerph15081650
- Hill CE, Myers JP, Vandenberg LN. Nonmonotonic dose-response curves occur in dose ranges that are relevant to regulatory decision-making. Dose Response. (2018) 16:1559325818798282. doi: 10.1177/1559325818798282
- Vandenberg LN. Low-dose effects of hormones and endocrine disruptors. In: Vitamins and Hormones (Elsevier Inc.). p. 129–165. doi: 10.1016/B978-0-12-800095-3.00005-5
- Mnif W, Ibn A, Hassine H, Bouaziz A, Bartegi A, Thomas O. Effect of endocrine disruptor pesticides: a review. Int J Environ Res Public Health. (2011) 8:2265–303. doi: 10.3390/ijerph8062265
- Bretveld RW, Thomas CMG, Scheepers PTJ, Zielhuis GA, Roeleveld N. Pesticide exposure: The hormonal function of the female reproductive system disrupted? Reprod Biol Endocrinol. (2006) 4:1–14. doi: 10.1186/1477-7827-4-30
- WHO. State-of-the-Science of Endocrine Disrupting Chemicals, 2012. United Nations Environment Programme and the World Health Organization, Geneva (2012).
- Burggren WW, Mueller CA. Developmental critical windows and sensitive periods as three-dimensional constructs in time and space. Physiol Biochem Zool. (2015) 88:91–102. doi: 10.1086/679906
- Fudvoye J, Bourguignon JP, Parent AS. Endocrine-disrupting chemicals and human growth and maturation: a focus on early critical windows of exposure. Vitam Horm. (2014) 94:1–25. doi: 10.1016/B978-0-12-800095-3.00001-8
- Sohmer H, Freeman S. The importance of thyroid hormone for auditory development in the fetus and neonate. Audiol Neurotol. (1996) 1:137–47. doi: 10.1159/000259194
- Kadenbach B, Freund R, Barth J, Akgün R, Linder D, Goglia F. Regulation of electron transport and proton pumping of cytochrome C oxidase by nucleotides and thyroid hormones. Prog Cell Res. (1995) 5:19–23. doi: 10.1016/B978-0-444-82235-2.50008-4
- Bernal J. Thyroid hormone receptors in brain development and function. Nat Clin Pract Endocrinol Metab. (2007) 3:249–59. doi: 10.1038/ncpendmet0424
- Korevaar TIM, Muetzel R, Medici M, Chaker L, Jaddoe VWV, de Rijke YB, et al. Association of maternal thyroid function during early pregnancy with offspring IQ and brain morphology in childhood: A population-based prospective cohort study. Lancet Diabetes Endocrinol. (2016) 4:35–43. doi: 10.1016/S2213-8587(15)00327-7
- Bellanger M, Demeneix B, Grandjean P, Zoeller RT, Trasande L. Neurobehavioral deficits, diseases, and associated costs of exposure to endocrine-disrupting chemicals in the European Union. J Clin Endocrinol Metab. (2015) 100:1256–66. doi: 10.1210/jc.2014-4323
- WHO. State-of-the-Science of Endocrine Disrupting Chemicals, 2012. United Nations Environment Programme and the World Health Organization, Geneva (2012).
- Bellanger M, Demeneix B, Grandjean P, Zoeller RT, Trasande L. Neurobehavioral deficits, diseases, and associated costs of exposure to endocrine-disrupting chemicals in the European Union. J Clin Endocrinol Metab. (2015) 100:1256–66. doi: 10.1210/jc.2014-4323
- Boas M, Feldt-rasmussen U, Main KM. Molecular and cellular endocrinology thyroid effects of endocrine disrupting chemicals. Mol Cell Endocrinol. (2012) 355:240–8. doi: 10.1016/j.mce.2011.09.005
- Crofton KM, Foss JA, Hass U, Jensen KF, Levin ED, Parker SP. Undertaking positive control studies as part of developmental neurotoxicity testing A report from the ILSI Research Foundation /Risk Science Institute expert working group on neurodevelopmental endpoints. Neurotoxicol Teratol. (2008) 30:266–87. doi: 10.1016/j.ntt.2007.06.002
- Diamanti-Kandarakis E, Bourguignon JP, Giudice LC, Hauser R, Prins GS, Soto AM, et al. Endocrine-disrupting chemicals: an Endocrine Society scientific statement. Endocr Rev. (2009) 30:293–342. doi: 10.1210/er.2009-0002
- European Food Safety Authority (EFSA). Scientific Opinion on the identification of pesticides to be included in cumulative assessment groups on the basis of their toxicological profile. EFSA J. (2013) 11:3293. doi: 10.2903/sp.efsa.2014.EN-538
- Brouwer A, Morse DC, Lans MC, Gerlienke Schuur A, Murk AJ, Klasson-Wehler E, et al. Interactions of persistent environmental organohalogens with the thyroid hormone system: mechanisms and possible consequences for animal and human health. Toxicol Ind Health. (1998) 14:59–84. doi: 10.1177/074823379801400107
- Mughal BB, Fini JB, Demeneix BA. Thyroid-disrupting chemicals and brain development: an update. Endocr Connect. (2018) 7:R160–86. doi: 10.1530/EC-18-0029
- Pleština R. Pesticides and herbicides|types of pesticide. In: Trugo L, Finglas PM, editors. Encyclopedia of Food Sciences and Nutrition. Baltimore, MD: Johns Hopkins University, Center for Human Nutrition, School of Hygiene and Public Health; Elsevier. p. 4473–4483. doi: 10.1016/B0-12-227055-X/00909-3
- US EPA. DDT – A Brief History and Status. (2012) Available online at: https://www.epa.gov/ingredients-used-pesticide-products/ddt-brief-history-and-status
- Carson R, Darling L, Darling L. Silent Spring. Boston, MA; Cambridge, MA: Houghton Mifflin Company; The Riverside Press (1962).
- Rogan WJ, Chen A. Health risks and benefits of bis(4-chlorophenyl)-1,1,1-trichloroethane (DDT). Lancet. (2005)763–73. doi: 10.1016/S0140-6736(05)67182-6
- Dietz R, Riget F, Cleemann M, Aarkrog A, Johansen P. Comparison of contaminants from different trophic levels and ecosystems. (2000) 245:221–31. doi: 10.1016/S0048-9697(99)00447-7
- Puertas R, Lopez-Espinosa MJ, Cruz F, Ramos R, Freire C, Pérez-García M, et al. Prenatal exposure to mirex impairs neurodevelopment at age of 4 years. Neurotoxicology. (2010) 31:154–60. doi: 10.1016/j.neuro.2009.09.009
- Torres-Sánchez L, Rothenberg SJ, Schnaas L, Cebrián ME, Osorio E, Carmen Hernández M, et al. In utero p,p′-DDE exposure and infant neurodevelopment-a perinatal cohort in Mexico. Environ Health Perspect. (2007) 115:435–9. doi: 10.1289/ehp.9566
- Gaspar FW, Harley KG, Kogut K, Chevrier J, Maria A, Sjödin A, et al. Prenatal DDT and DDE exposure and child IQ in the CHAMACOS cohort. Environ Int. (2015) 85:206–12. doi: 10.1016/j.envint.2015.09.004
- Agency for Toxic Substances and Disease Registry (ATSDR). Toxicological Profile for DDT, DDE, and DDD. (2002). Available online at: https://www.atsdr.cdc.gov/toxprofiles/tp35.pdf
- Berghuis SA, Bos AF, Sauer PJ, Roze E. Developmental neurotoxicity of persistent organic pollutants: an update on childhood outcome. Arch Toxicol. (2015) 89:687–709. doi: 10.1007/s00204-015-1463-3
- Roze E, Meijer L, Bakker A, Van Braeckel KNJA, Sauer PJJ, Bos AF. Prenatal exposure to organohalogens, including brominated flame retardants, influences motor, cognitive, and behavioral performance at school age. Environ Health Perspect. (2009) 117:1953–8. doi: 10.1289/ehp.0901015
- Torres-Sánchez L, Schnaas L, Cebrián ME, Hernández MC, Valencia EO, García Hernández RM, et al. Prenatal dichlorodiphenyldichloroethylene (DDE) exposure and neurodevelopment: A follow-up from 12 to 30 months of age. Neurotoxicology. (2009) 30:1162–5. doi: 10.1016/j.neuro.2009.08.010
- Sagiv SK, Thurston SW, Bellinger DC, Tolbert PE, Altshul LM, Korrick SA. Prenatal organochlorine exposure and behaviors associated with attention deficit hyperactivity disorder in school-aged children. Am J Epidemiol. (2010) 171:593–601. doi: 10.1093/aje/kwp427
- Ribas-Fitó N, Torrent M, Carrizo D, Júlvez J, Grimalt JO, Sunyer J. Exposure to hexachlorobenzene during pregnancy and children’s social behavior at 4 years of age. Environ Health Perspect. (2007) 115:447–50. doi: 10.1289/ehp.9314
- Sioen I, Den Hond E, Nelen V, Van de Mieroop E, Croes K, Van Larebeke N, et al. Prenatal exposure to environmental contaminants and behavioural problems at age 7 – 8 years. Environ Int. (2013) 59:225–31. doi: 10.1016/j.envint.2013.06.014
- Alvarez-Pedrerol M, Carrizo D, Grimalt JO, Sunyer J. Effects of PCBs, p,p′-DDT, p,p′-DDE, HCB and β-HCH on thyroid function in preschool children. Occup Environ Med. (2008) 65:452–7. doi: 10.1136/oem.2007.032763
- Asawasinsopon R, Prapamontol T, Prakobvitayakit O, Vaneesorn Y. The association between organochlorine and thyroid hormone levels in cord serum: a study from northern Thailand. Environ Int. (2006) 32:554–9. doi: 10.1016/j.envint.2006.01.001
- 72. Lopez-Espinosa MJ, Vizcaino E, Murcia M, Fuentes V, Garcia AM, Rebagliato M, et al. Prenatal exposure to organochlorine compounds and neonatal thyroid stimulating hormone levels. J Expo Sci Environ Epidemiol. (2009) 20:579–88. doi: 10.1038/jes.2009.47
- Ribas-Fitó N, Sala M, Cardo E, Mazón C, De Muga ME, Verdú A, et al. Organochlorine compounds and concentrations of thyroid stimulating hormone in newborns. Occup Environ Med. (2003) 60:301–3. doi: 10.1136/oem.60.4.301
- Dallaire R, Dewailly É, Ayotte P, Muckle G, Laliberté C, Bruneau S. Effects of prenatal exposure to organochlorines on thyroid hormone status in newborns from two remote coastal regions in Québec, Canada. Environ Res. (2008) 108:387–92. doi: 10.1016/j.envres.2008.08.004
- Freire C, Lopez-espinosa M, Fernández M, Molina-molina J. Science of the total environment prenatal exposure to organochlorine pesticides and TSH status in newborns from. Sci Total Environ. (2011) 409:3281–7. doi: 10.1016/j.scitotenv.2011.05.037
- Kim S, Park J, Kim HJ, Lee JJ, Choi G, Choi S, et al. Association between several persistent organic pollutants and thyroid hormone levels in cord blood serum and bloodspot of the newborn infants of Korea. PLoS ONE. (2015) 10:e0125213. doi: 10.1371/journal.pone.0125213
- Luo D, Pu Y, Tian H, Wu W, Sun X, Zhou T, et al. Association of in utero exposure to organochlorine pesticides with thyroid hormone levels in cord blood of newborns. Environ Pollut. (2017) 231:78–86. doi: 10.1016/j.envpol.2017.07.091
- 78. Takser L, Mergler D, Baldwin M, de Grosbois S, Smargiassi A, Lafond J. Thyroid hormones in pregnancy in relation to environmental exposure to organochlorine compounds and mercury. Environ Health Perspect. (2005) 113:1039–45. doi: 10.1289/ehp.7685
- Maervoet J, Vermeir G, Covaci A, Van Larebeke N, Koppen G, Schoeters G, et al. Association of thyroid hormone concentrations with levels of organochlorine compounds in cord blood of neonates. Environ Health Perspect. (2007) 115:1780–6. doi: 10.1289/ehp.10486
- Cordier S, Bouquet E, Warembourg C, Massart C, Rouget F, Kadhel P, et al. Perinatal exposure to chlordecone, thyroid hormone status and neu- rodevelopment in infants: The Timoun cohort study in Guadeloupe (French West Indies). Environ Res. (2015) 138:271–8. doi: 10.1016/j.envres.2015.02.021
- Dufour P, Pirard C, Seghaye MC, Charlier C. Association between organohalogenated pollutants in cord blood and thyroid function in newborns and mothers from Belgian population. Environ Pollut. (2018) 238:389–96. doi: 10.1016/j.envpol.2018.03.058
- Dallaire R, Dewailly É, Ayotte P, Muckle G, Laliberté C, Bruneau S. Effects of prenatal exposure to organochlorines on thyroid hormone status in newborns from two remote coastal regions in Québec, Canada. Environ Res. (2008) 108:387–92. doi: 10.1016/j.envres.2008.08.004
- Cordier S, Bouquet E, Warembourg C, Massart C, Rouget F, Kadhel P, et al. Perinatal exposure to chlordecone, thyroid hormone status and neu- rodevelopment in infants: The Timoun cohort study in Guadeloupe (French West Indies). Environ Res. (2015) 138:271–8. doi: 10.1016/j.envres.2015.02.021
- Blanco-muñoz J, Lacasaña M, López-flores I, Rodríguez-barranco M, González-alzaga B, Bassol S, et al. Association between organochlorine pesticide exposure and thyroid hormones in floriculture workers. Environ Res. (2016) 150:357–63. doi: 10.1016/j.envres.2016.05.054
- Rathore M, Bhatnagar P, Mathur D, Saxena GN. Burden of organochlorine pesticides in blood and its effect on thyroid hormones in women. Sci Total Environ. (2002) 295:207–15. doi: 10.1016/S0048-9697(02)00094-3
- Rylander L, Wallin E, Jönssson BA, Stridsberg M, Erfurth EM, Hagmar L. Associations between CB-153 and p,p′-DDE and hormone levels in serum in middle-aged and elderly men. Chemosphere. (2006) 65:375–81. doi: 10.1016/j.chemosphere.2006.02.012
- Schell LM, Gallo MV, Denham M, Ravenscroft J, DeCaprio AP, Carpenter DO. Relationship of thyroid hormone levels to levels of polychlorinated biphenyls, lead, p,p’-DDE, and other toxicants in Akwesasne Mohawk Youth. Environ Health Perspect. (2008) 116:806–13. doi: 10.1289/ehp.10490
- Goldner WS, Sandler DP, Yu F, Hoppin JA, Kamel F, Levan TD. Pesticide use and thyroid disease among women in the Agricultural Health Study. Am J Epidemiol. (2010) 171:455–64. doi: 10.1093/aje/kwp404
- Goldner WS, Sandler DP, Yu F, Shostrom V, Hoppin JA, Kamel F, et al. Hypothyroidism and pesticide use among male private pesticide applicators in the agricultural health study. J Occup Environ Med. (2013) 55:1171–8. doi: 10.1097/JOM.0b013e31829b290b
- Piccoli C, Cremonese C, Koifman RJ, Koifman S, Freire C. Pesticide exposure and thyroid function in an agricultural population in Brazil. Environ Res. (2016) 151:389–98. doi: 10.1016/j.envres.2016.08.011
- Shrestha S, Parks CG, Goldner WS, Kamel F, Umbach DM, Ward MH, et al. Pesticide use and incident hypothyroidism in pesticide applicators in the Agricultural Health Study. Environ Health Perspect. (2018) 126:97008. doi: 10.1289/EHP3194
- Lerro CC, Beane Freeman LE, DellaValle CT, Kibriya MG, Aschebrook-Kilfoy B, Jasmine F, et al. Occupational pesticide exposure and subclinical hypothyroidism among male pesticide applicators. Occup Environ Med. (2018) 75:79–89. doi: 10.1136/oemed-2017-104431
- Agency for Toxic Substances and Disease Registry (ATSDR). Toxicological Profile for DDT, DDE, and DDD. (2002). Available online at: https://www.atsdr.cdc.gov/toxprofiles/tp35.pdf
- Liu C, Shi Y, Li H, Wang Y, Yang K. p,p ′-DDE disturbs the homeostasis of thyroid hormones via thyroid hormone receptors, transthyretin, and hepatic enzymes. Horm Metab Res. (2011) 43:391–6. doi: 10.1055/s-0031-1277135
- Langer P. The impacts of organochlorines and other persistent pollutants on thyroid and metabolic health. Front Neuroendocrinol. (2010) 31:497–518. doi: 10.1016/j.yfrne.2010.08.001
- Alvarez L, Hernández S, Martinez-de-Mena R, Kolliker-Frers R, Obregón MJ, Kleiman de Pisarev DL. The role of type I and type II 5′ deiodinases on hexachlorobenzene-induced alteration of the hormonal thyroid status. Toxicology. (2005) 207:349–62. doi: 10.1016/j.tox.2004.10.006
- van Raaij JA, Frijters CM, van den Berg KJ. Hexachlorobenzene-induced hypothyroidism. Involvement of different mechanisms by parent compound and metabolite. Biochem Pharmacol. (1993) 46:1385–91. doi: 10.1016/0006-2952(93)90103-4
- Starek-Świechowicz B, Budziszewska B, Starek A. Hexachlorobenzene as a persistent organic pollutant: Toxicity and molecular mechanism of action. Pharmacol Rep. (2017) 69:1232–9. doi: 10.1016/j.pharep.2017.06.013
- Yaglova NV, Yaglov VV. Changes in thyroid status of rats after prolonged exposure to low dose dichlorodiphenyltrichloroethane. Bull Exp Biol Med. (2014) 156:760–2. doi: 10.1007/s10517-014-2443-y
- Yaglova NV, Yaglov VV. Cytophysiological changes in the follicular epithelium of the thyroid gland after long-term exposure to low doses of dichlorodiphenyltrichloroethane (DDT). Bull Exp Biol Med. (2017) 162:699–702. doi: 10.1007/s10517-017-3691-4
- Santini F, Vitti P, Ceccarini G, Mammoli C, Rosellini V, Pelosini C, et al. In vitro assay of thyroid disruptors affecting TSH-stimulated adenylate cyclase activity. J Endocrinol Invest. (2003) 26:950–5. doi: 10.1007/BF03348190
- Rossi M, Dimida A, Dell’anno MT, Trincavelli ML, Agretti P, Giorgi F, et al. The thyroid disruptor 1,1,1-trichloro-2,2-bis(p-chlorophenyl)-ethane appears to be an uncompetitive inverse agonist for the thyrotropin receptor. J Pharmacol Exp Ther. (2006) 320:465–74. doi: 10.1124/jpet.106.113613
- Rossi M, Taddei AR, Fasciani I, Maggio R, Giorgi F. The cell biology of the thyroid-disrupting mechanism of dichlorodiphenyltrichloroethane (DDT). J Endocrinol Invest. (2018) 41:67–73. doi: 10.1007/s40618-017-0716-9
- Chiappini F, Pontillo C, Randi A, Alvarez L, Kleiman de Pisarev DL. Hexachlorobenzene induces TGF-β1 expression, which is a regulator of p27 and cyclin D1 modifications. Toxicol Lett. (2014) 230:1–9. doi: 10.1016/j.toxlet.2014.08.002
- Nicolussi A, D’Inzeo S, Santulli M, Colletta G, Coppa A. TGF-β control of rat thyroid follicular cells differentiation. Mol Cell Endocrinol. (2003) 207:1–11. doi: 10.1016/S0303-7207(03)00238-7
- Vale A. Organophosphorus insecticide poisoning. BMJ Clin Evid. (2015) 2015:2102.
- Rauh VA, Whyatt RM, Perera FP, Horton MK, Hao X, Barr DB, et al. Brain anomalies in children exposed prenatally to a common organophosphate pesticide. Proc Natl Acad Sci USA. (2012) 109:7871–6. doi: 10.1073/pnas.1203396109
- Qiao D, Seidler FJ, Padilla S, Slotkin TA. Developmental neurotoxicity of chlorpyrifos: What is the vulnerable period? Environ Health Perspect. (2002) 110:1097–103. doi: 10.1289/ehp.021101097
- Trasande L. When enough data are not enough to enact policy: The failure to ban chlorpyrifos. PLoS Biol. (2017) 15:e2003671. doi: 10.1371/journal.pbio.2003671
- Suhartono S, Kartini A, Subagio HW, Budiyono B, Utari A, Suratman S, et al. Pesticide exposure and thyroid function in elementary school children living in an agricultural area, Brebes District, Indonesia. Int J Occup Environ Med. (2018) 9:137–44. doi: 10.15171/ijoem.2018.1207
- Shrestha S, Parks CG, Goldner WS, Kamel F, Umbach DM, Ward MH, et al. Pesticide use and incident hypothyroidism in pesticide applicators in the Agricultural Health Study. Environ Health Perspect. (2018) 126:97008. doi: 10.1289/EHP3194
- Huang HS, Lee KW, Ho CH, Hsu CC, Su SB, Wang JJ, et al. Increased risk for hypothyroidism after anticholinesterase pesticide poisoning: a nationwide population-based study. Endocrine. (2017) 57:436–44. doi: 10.1007/s12020-017-1373-7
- Medda E, Santini F, De Angelis S, Franzellin F, Fiumalbi C, Perico A, et al. Iodine nutritional status and thyroid effects of exposure to ethylenebisdithiocarbamates. Environ Res. (2017) 154:152–9. doi: 10.1016/j.envres.2016.12.019
- Rauh VA, Whyatt RM, Perera FP, Horton MK, Hao X, Barr DB, et al. Brain anomalies in children exposed prenatally to a common organophosphate pesticide. Proc Natl Acad Sci USA. (2012) 109:7871–6. doi: 10.1073/pnas.1203396109
- Bouchard MF, Kogut K, Barr DB, Eskenazi B, Bradman A, Vedar M, et al. Prenatal exposure to organophosphate pesticides and IQ in 7-year-old children. Environ Health Perspect. (2011) 119:1189–95. doi: 10.1289/ehp.1003185
- Lerro CC, Koutros S, Andreotti G, Friesen MC, Alavanja MC, Blair A, et al. Organophosphate insecticide use and cancer incidence among spouses of pesticide applicators in the Agricultural Health Study. Occup Environ Med. (2015) 72:736–44. doi: 10.1136/oemed-2014-102798
- Bouchard MF, Kogut K, Barr DB, Eskenazi B, Bradman A, Vedar M, et al. Prenatal exposure to organophosphate pesticides and IQ in 7-year-old children. Environ Health Perspect. (2011) 119:1189–95. doi: 10.1289/ehp.1003185
- Rauh VA, Whyatt RM, Perera FP, Horton MK, Hao X, Barr DB, et al. Brain anomalies in children exposed prenatally to a common organophosphate pesticide. Proc Natl Acad Sci USA. (2012) 109:7871–6. doi: 10.1073/pnas.1203396109
- Suhartono S, Kartini A, Subagio HW, Budiyono B, Utari A, Suratman S, et al. Pesticide exposure and thyroid function in elementary school children living in an agricultural area, Brebes District, Indonesia. Int J Occup Environ Med. (2018) 9:137–44. doi: 10.15171/ijoem.2018.1207
- Lerro CC, Koutros S, Andreotti G, Friesen MC, Alavanja MC, Blair A, et al. Organophosphate insecticide use and cancer incidence among spouses of pesticide applicators in the Agricultural Health Study. Occup Environ Med. (2015) 72:736–44. doi: 10.1136/oemed-2014-102798
- Wang Y, Chen L, Wang C, Hum Y, Gao Y, Zhou Y, et al. Association between organophosphate pesticide exposure and thyroid hormones in pregnant women. Epidemiology. (2017) 28(Suppl. 1):S35–40. doi: 10.1097/EDE.0000000000000721
- De Angelis S, Tassinari R, Maranghi F, Eusepi A, Di Virgilio A, Chiarotti F, et al. Developmental exposure to chlorpyrifos induces alterations in thyroid and thyroid hormone levels without other toxicity signs in CD-1 mice. Toxicol Sci. (2009) 108:311–9. doi: 10.1093/toxsci/kfp017
- Wilson NK, Chuang JC, Lyu C, Menton R, Morgan MK. Aggregate exposures of nine preschool children to persistent organic pollutants at day care and at home. J Expo Anal Environ Epidemiol. (2003) 13:187–202. doi: 10.1038/sj.jea.7500270
- Mie A, Rudén C, Grandjean P. Safety of Safety Evaluation of Pesticides: developmental neurotoxicity of chlorpyrifos and chlorpyrifos-methyl. Environ Health. (2018) 17:77. doi: 10.1186/s12940-018-0421-y
- Holzer G, Besson M, Lambert A, Francois L, Barth P, Gillet B, et al. Fish larval recruitment to reefs is a thyroid hormone-mediated metamorphosis sensitive to the pesticide chlorpyrifos. Elife. (2017) 6:e27595. doi: 10.7554/eLife.27595
- Zhang X, Tian H, Wang W, Ru S. Monocrotophos pesticide decreases the plasma levels of total 3,3′,5-triiodo-l-thyronine and alters the expression of genes associated with the thyroidal axis in female goldfish (Carassius auratus). PLoS ONE. (2014) 9:e108972. doi: 10.1371/journal.pone.0108972
- Zhang X, Liu W, Wang J, Tian H, Wang W, Ru S. Quantitative analysis of in-vivo responses of reproductive and thyroid endpoints in male goldfish exposed to monocrotophos pesticide. Comp Biochem Physiol C Toxicol Pharmacol. (2018) 211:41–7. doi: 10.1016/j.cbpc.2018.05.010
- Katuli KK, Amiri BM, Massarsky A, Yelghi S. Impact of a short-term diazinon exposure on the osmoregulation potentiality of Caspian roach (Rutilus rutilus) fingerlings. Chemosphere. (2014) 108:396–404. doi: 10.1016/j.chemosphere.2014.02.038
- Ortiz-Delgado JB, Funes V, Sarasquete C. The organophosphate pesticide -OP- malathion inducing thyroidal disruptions and failures in the metamorphosis of the Senegalese sole, Solea senegalensis. BMC Vet Res. (2019) 15:57. doi: 10.1186/s12917-019-1786-z
- Benbrook CM. Trends in glyphosate herbicide use in the United States and globally. Environ Sci Eur. (2016) 28:3. doi: 10.1186/s12302-016-0070-0
- Shrestha S, Parks CG, Goldner WS, Kamel F, Umbach DM, Ward MH, et al. Pesticide use and incident hypothyroidism in pesticide applicators in the Agricultural Health Study. Environ Health Perspect. (2018) 126:97008. doi: 10.1289/EHP3194
- Goldner WS, Sandler DP, Yu F, Shostrom V, Hoppin JA, Kamel F, et al. Hypothyroidism and pesticide use among male private pesticide applicators in the agricultural health study. J Occup Environ Med. (2013) 55:1171–8. doi: 10.1097/JOM.0b013e31829b290b
- Lerro CC, Beane Freeman LE, DellaValle CT, Kibriya MG, Aschebrook-Kilfoy B, Jasmine F, et al. Occupational pesticide exposure and subclinical hypothyroidism among male pesticide applicators. Occup Environ Med. (2018) 75:79–89. doi: 10.1136/oemed-2017-104431
- de Souza JS, Kizys MML, da Conceicao RR, Glebocki G, Romano RM, Ortiga-Carvalho TM, et al. Perinatal exposure to glyphosate-based herbicide alters the thyrotrophic axis and causes thyroid hormone homeostasis imbalance in male rats. Toxicology. (2017) 377:25–37. doi: 10.1016/j.tox.2016.11.005
- Howe CM, Berrill M, Pauli BD, Helbing CC, Werry K, Veldhoen N. Toxicity of glyphosate-based pesticides to four north American frog species. Environ Toxicol Chem. (2004) 23:1928–38. doi: 10.1897/03-71
- Lanctot C, Navarro-Martin L, Robertson C, Park B, Jackman P, Pauli BD, et al. Effects of glyphosate-based herbicides on survival, development, growth and sex ratios of wood frog (Lithobates sylvaticus) tadpoles. II: agriculturally relevant exposures to Roundup WeatherMax(R) and Vision(R) under laboratory conditions. Aquat Toxicol. (2014) 154:291–303. doi: 10.1016/j.aquatox.2014.05.025
- Colovic MB, Krstic DZ, Lazarevic-Pasti TD, Bondzic AM, Vasic VM. Acetylcholinesterase inhibitors: pharmacology and toxicology. Curr Neuropharmacol. (2013) 11:315–35. doi: 10.2174/1570159X11311030006
- Houeto P, Bindoula G, Hoffman JR. Ethylenebisdithiocarbamates and ethylenethiourea: possible human health hazards. Environ Health Perspect. (1995) 103:568–73. doi: 10.1289/ehp.95103568
- Hedenstedt A, Rannug U, Ramel C, Wachtmeister CA. Mutagenicity and metabolism studies on 12 thiuram and dithiocarbamate compounds used as accelerators in the Swedish rubber industry. Mutat Res Toxicol. (1979) 68:313–25. doi: 10.1016/0165-1218(79)90164-2
- Davidson B, Soodak M, Strout HV, Neary JT, Nakamura C, Maloof F. Thiourea and cyanamide as inhibitors of thyroid peroxidase: the role of iodide*. Endocrinology. (1979) 104:919–24. doi: 10.1210/endo-104-4-919
- Jardim ANO, Mello DC, Brito AP, van der Voet H, Boon PE, Caldas ED. Probabilistic dietary risk assessment of triazole and dithiocarbamate fungicides for the Brazilian population. Food Chem Toxicol. (2018) 118:317–27. doi: 10.1016/j.fct.2018.05.002
- Huang HS, Lee KW, Ho CH, Hsu CC, Su SB, Wang JJ, et al. Increased risk for hypothyroidism after anticholinesterase pesticide poisoning: a nationwide population-based study. Endocrine. (2017) 57:436–44. doi: 10.1007/s12020-017-1373-7
- Medda E, Santini F, De Angelis S, Franzellin F, Fiumalbi C, Perico A, et al. Iodine nutritional status and thyroid effects of exposure to ethylenebisdithiocarbamates. Environ Res. (2017) 154:152–9. doi: 10.1016/j.envres.2016.12.019
- Laisi A, Tuominen R, Männistö P, Savolainen K, Mattila J. The effect of maneb, zineb, and ethylenethiourea on the humoral activity of the pituitary-thyroid axis in rat. Arch Toxicol Suppl. (1985) 8:253–8. doi: 10.1007/978-3-642-69928-3_37
- Pandey SP, Mohanty B. The neonicotinoid pesticide imidacloprid and the dithiocarbamate fungicide mancozeb disrupt the pituitary-thyroid axis of a wildlife bird. Chemosphere. (2015) 122:227–34. doi: 10.1016/j.chemosphere.2014.11.061
- Kackar R, Srivastava MK, Raizada RB. Studies on rat thyroid after oral administration of mancozeb: morphological and biochemical evaluations. J Appl Toxicol. (1997) 17:369–75.
- Marinovich M, Guizzetti M, Ghilardi F, Viviani B, Corsini E, Galli CL. Thyroid peroxidase as toxicity target for dithiocarbamates. Arch Toxicol. (1997) 71:508–12. doi: 10.1007/s002040050420
- Chernick M, Yu Y, Teraoka H, Nanba S, Hinton DE, Wang F, et al. The case for thyroid disruption in early life stage exposures to thiram in zebrafish (Danio rerio). Gen Comp Endocrinol. (2018) 271:73–81. doi: 10.1016/j.ygcen.2018.11.003
- Elliott M, Farnham AW, Janes NF, Khambay BPS. Insecticidal activity of the pyrethrins and related compounds. Part XII: α-substituted-3-phenoxybenzyl esters. Pestic Sci. (1982) 13:407–14. doi: 10.1002/ps.2780130411
- Anadón A, Martínez-Larrañaga MR, Martínez MA. Use and abuse of pyrethrins and synthetic pyrethroids in veterinary medicine. Vet J. (2009) 182:7–20. doi: 10.1016/j.tvjl.2008.04.008
- Elbert A, Haas M, Springer B, Thielert W, Nauen R. Applied aspects of neonicotinoid uses in crop protection. Pest Manag Sci. (2008) 64:1099–105. doi: 10.1002/ps.1616
- Juraske R, Mutel CL, Stoessel F, Hellweg S. Life cycle human toxicity assessment of pesticides: comparing fruit and vegetable diets in Switzerland and the United States. Chemosphere. (2009) 77:939–45. doi: 10.1016/j.chemosphere.2009.08.006
- Laskowski DA. Physieal and chemie al properties of pyrethroids. Rev Env Contam Toxieol. (2002) 174:49–170. doi: 10.1007/978-1-4757-4260-2_3
- Ge J, Cong J, Sun Y, Li G, Zhou Z, Qian C, Liu F. Determination of endocrine disrupting chemicals in surface water and industrial wastewater from Beijing, China. Bull Environ Contam Toxicol. (2010) 84:401–5. doi: 10.1007/s00128-010-9958-3
- Hladik ML, Kuivila KM. Assessing the occurrence and distribution of pyrethroids in water and suspended sediments. J Agric Food Chem. (2009) 57:9079–85. doi: 10.1021/jf9020448
- Zhang J, Yoshinaga J, Hisada A, Shiraishi H, Shimodaira K, Okai T, et al. Prenatal pyrethroid insecticide exposure and thyroid hormone levels and birth sizes of neonates. Sci Total Environ. (2014) 488–9:275–9. doi: 10.1016/j.scitotenv.2014.04.104
- Li Z, Nie J, Lu Z, Xie H, Kang L, Chen Q, et al. Cumulative risk assessment of the exposure to pyrethroids through fruits consumption in China – Based on a 3-year investigation. Food Chem Toxicol. (2016) 96:234–43. doi: 10.1016/j.fct.2016.08.012
- Du G, Shen O, Sun H, Fei J, Lu C, Song L, et al. Assessing hormone receptor activities of pyrethroid insecticides and their metabolites in reporter gene assays. Toxicol Sci. (2010) 116:58–66. doi: 10.1093/toxsci/kfq120
- Zhang J, Yoshinaga J, Hisada A, Shiraishi H, Shimodaira K, Okai T, et al. Prenatal pyrethroid insecticide exposure and thyroid hormone levels and birth sizes of neonates. Sci Total Environ. (2014) 488–9:275–9. doi: 10.1016/j.scitotenv.2014.04.104
- Du G, Shen O, Sun H, Fei J, Lu C, Song L, et al. Assessing hormone receptor activities of pyrethroid insecticides and their metabolites in reporter gene assays. Toxicol Sci. (2010) 116:58–66. doi: 10.1093/toxsci/kfq120
- Nassr ACC, Arena AC, Toledo FC, Bissacot DZ, Fernandez CDB, Spinardi-Barbisan ALT, et al. Effects of gestational and lactational fenvalerate exposure on immune and reproductive systems of male rats. J Toxicol Environ Heal A Curr Issues. (2010) 73:952–64. doi: 10.1080/15287391003751745
- Pérez JJ, Williams MK, Weerasekera G, Smith K, Whyatt RM, Needham LL, Barr DB. Measurement of pyrethroid, organophosphorus, and carbamate insecticides in human plasma using isotope dilution gas chromatography-high resolution mass spectrometry. J Chromatogr B Anal Technol Biomed Life Sci. (2010) 878:2554–62. doi: 10.1016/j.jchromb.2010.03.015
- Kaul PP, Rastogi A, Hans RK, Seth TD, Seth PK, Srimal RC. Fenvalerate-induced alterations in circulatory thyroid hormones and calcium stores in rat brain. Toxicol Lett. (1996) 89:29–33. doi: 10.1016/S0378-4274(96)03778-2
- Giray B, Cağlayan A, Erkekoğlu P, Hincal F. Fenvalerate exposure alters thyroid hormone status in selenium- and/or iodine-deficient rats. Biol Trace Elem Res. (2010) 135:233–41. doi: 10.1007/s12011-009-8506-7
- Wang B, Liu JJ, Wang Y, Fu L, Shen R, Yu Z, et al. Maternal fenvalerate exposure induces fetal intrauterine growth restriction through disrupting placental thyroid hormone receptor signaling. Toxicol Sci. (2017) 157:377–86. doi: 10.1093/toxsci/kfx052
- Chang J, Hao W, Xu Y, Xu P, Li W, Li J, Wang H. Stereoselective degradation and thyroid endocrine disruption of lambda-cyhalothrin in lizards (Eremias argus) following oral. Environ Pollut. (2017) 232:300–9. doi: 10.1016/j.envpol.2017.09.072
- Tu W, Xu C, Jin Y, Lu B, Lin C, Wu Y, Liu W. Permethrin is a potential thyroid-disrupting chemical: In vivo and in silico envidence. Aquat Toxicol. (2016) 175:39–46. doi: 10.1016/j.aquatox.2016.03.006
- Tu W, Xu C, Lu B, Lin C, Wu Y, Liu W. Acute exposure to synthetic pyrethroids causes bioconcentration and disruption of the hypothalamus-pituitary-thyroid axis in zebrafish embryos. Sci Total Environ. (2016) 542:876–85. doi: 10.1016/j.scitotenv.2015.10.131
- Xu C, Li X, Jin M, Sun X, Niu L, Lin C, et al. Early life exposure of zebrafish (Danio rerio) to synthetic pyrethroids and their metabolites: a comparison of phenotypic and behavioral indicators and gene expression involved in the HPT axis and innate immune system. Environ Sci Pollut Res Int. (2018) 25:12992–3003. doi: 10.1007/s11356-018-1542-0
- Giroux M, Gan J, Schlenk D. The Effects of bifenthrin and temperature on the endocrinology of Juvenile Chinook Salmon. Environ Toxicol Chem. (2019) 38:852–61. doi: 10.1002/etc.4372
- Tingle CCD, Rother JA, Dewhurst CF, Lauer S, King WJ. Fipronil: environmental fate, ecotoxicology, and human health concerns. In: Ware GW, editor. Reviews of Environmental Contamination and Toxicology. Reviews of Environmental Contamination and Toxicology. Vol. 176. New York, NY: Springer (2003). p. 1–66. doi: 10.1007/978-1-4899-7283-5_1
- Kim YA, Yoon YS, Kim HS, Jeon SJ, Cole E, Lee J, et al. Distribution of fipronil in humans, and adverse health outcomes of in utero fipronil sulfone exposure in newborns. Int J Hyg Environ Health. (2019) 222:524–32. doi: 10.1016/j.ijheh.2019.01.009
- Simon-Delso N, Amaral-Rogers V, Belzunces LP, Bonmatin JM, Chagnon M, Downs C, et al. Systemic insecticides (neonicotinoids and fipronil): trends, uses, mode of action and metabolites. Environ Sci Pollut Res. (2015) 22:5–34. doi: 10.1007/s11356-014-3470-y
- Stone WW, Gilliom RJ, Ryberg KR. Pesticides in U.S. Streams and Rivers: Occurrence and Trends during 1992–2011. Environ Sci Technol. (2014) 48:11025–30. doi: 10.1021/es5025367
- Bonmatin J, Giorio C, Girolami V, Goulson D, Kreutzweiser DP. Environmental fate and exposure; neonicotinoids and fipronil. Environ Sci Pollut Res Int. (2015) 22:35–67. doi: 10.1007/s11356-014-3332-7
- Mahler BJ, Van Metre PC, Wilson JT, Musgrove M, Zaugg SD, Burkhardt MR. Fipronil and its degradates in indoor and outdoor dust. Environ Sci Technol. (2009) 43:5665–70. doi: 10.1021/es901292a
- Li X, Li H, Ma W, Guo Z, Li X, Song S, Tang H. Development of precise GC-EI-MS method to determine the residual fi pronil and its metabolites in chicken egg. Food Chem. (2019) 281:85–90. doi: 10.1016/j.foodchem.2018.12.041
- Fipronil Egg Scandal: What We Know – BBC News. (2017). Available online at: https://www.bbc.com/news/world-europe-40878381
- Holder PJ, Jones A, Tyler CR, Cresswell JE. Fipronil pesticide as a suspect in historical mass mortalities of honey bees. Proc Natl Acad Sci USA. (2018) 115:13033–8. doi: 10.1073/pnas.1804934115
- General Court of the European Union. General Court of the European Union Press Release No 68/18 The General Court Confirms the Validity of the Restrictions Introduced at EU Level in 2013 Against the Insecticides Clothianidin, Thiamethoxam and Imidacloprid Because of the Risks Those Substa. (2018).
- Tingle CCD, Rother JA, Dewhurst CF, Lauer S, King WJ. Fipronil: environmental fate, ecotoxicology, and human health concerns. In: Ware GW, editor. Reviews of Environmental Contamination and Toxicology. Reviews of Environmental Contamination and Toxicology. Vol. 176. New York, NY: Springer (2003). p. 1–66. doi: 10.1007/978-1-4899-7283-5_1
- Wang X, Martínez MA, Wu Q, Ares I, Martínez-Larrañaga MR, Anadón A, et al. Fipronil insecticide toxicology: oxidative stress and metabolism. Crit Rev Toxicol. (2016) 46:876–99. doi: 10.1080/10408444.2016.1223014
- Hainzl D, Cole LM, Casida JE. Mechanisms for selective toxicity of fipronil insecticide and its sulfone metabolite and desulfinyl photoproduct. Chem Res Toxicol. (1998) 11:1529–35. doi: 10.1021/tx980157t
- Gunasekara AS, Truong T, Goh KS, Spurlock F, Tjeerdema RS. Environmental fate and toxicology of fipronil. J Pestic Sci. (2007) 32:189–99. doi: 10.1584/jpestics.R07-02
- Lacroix MZ, Puel S, Toutain PL, Viguié C. Quantification of fipronil and its metabolite fipronil sulfone in rat plasma over a wide range of concentrations by LC/UV/MS. J Chromatogr B Analyt Technol Biomed Life Sci. (2010) 878:1934–8. doi: 10.1016/j.jchromb.2010.05.018
- Konwick BJ, Garrison AW, Black MC, Avants JK, Fisk AT. Bioaccumulation, biotransformation, and metabolite formation of fipronil and chiral legacy pesticides in rainbow trout. Environ Sci Technol. (2006) 40:2930–6. doi: 10.1021/es0600678
- Romero A, Ramos E, Ares I, Castellano V, Martínez M, Anadón A, Martínez MA. Fipronil sulfone induced higher cytotoxicity than fi pronil in SH-SY5Y cells: protection by antioxidants. Toxicol Lett. (2016) 252:42–9. doi: 10.1016/j.toxlet.2016.04.005
- Leghait J, Gayrard V, Picard-Hagen N, Camp M, Perdu E, Toutain PL, et al. Fipronil-induced disruption of thyroid function in rats is mediated by increased total and free thyroxine clearances concomitantly to increased activity of hepatic enzymes. Toxicology. (2009) 255:38–44. doi: 10.1016/j.tox.2008.09.026
- Roques BB, Lacroix MZ, Puel S, Gayrard V, Picard-Hagen N, Jouanin I, et al. CYP450-Dependent biotransformation of the insecticide fipronil into fipronil sulfone can mediate fipronil-induced thyroid disruption in rats. Toxicol Sci. (2012) 127:29–41. doi: 10.1093/toxsci/kfs094
- Mohamed F, Senarathna L, Percy A, Abeyewardene M, Eaglesham G, Cheng R, et al. Acute human self-poisoning with the N-phenylpyrazole insecticide fipronil—a GABA A gated chloride channel blocker. J Toxicol Clin Toxicol. (2004) 42:955–63. doi: 10.1081/CLT-200041784
- Herin F, Boutet-robinet E, Levant A, Dulaurent S, Manika M, Galatry-bouju F, et al. Thyroid function tests in persons with occupational exposure to fipronil. Thyroid. (2011) 21: 701–6. doi: 10.1089/thy.2010.0449
- Kim YA, Yoon YS, Kim HS, Jeon SJ, Cole E, Lee J, et al. Distribution of fipronil in humans, and adverse health outcomes of in utero fipronil sulfone exposure in newborns. Int J Hyg Environ Health. (2019) 222:524–32. doi: 10.1016/j.ijheh.2019.01.009
- Razaz N, Boyce WT, Brownell M, Jutte D, Tremlett H, Marrie RA, et al. Five-minute Apgar score as a marker for developmental vulnerability at 5 years of age. Arch Dis Child Fetal Neonatal Ed. (2016) 101:F114–20. doi: 10.1136/archdischild-2015-308458
- Hurley PM, Hill RN, Whiting RJ. Mode of carcinogenic action of pesticides inducing thyroid follicular cell tumors in rodents. Environ Health Perspect. (1998) 106:437–45. doi: 10.1289/ehp.98106437
- Leghait J, Gayrard V, Picard-Hagen N, Camp M, Perdu E, Toutain PL, et al. Fipronil-induced disruption of thyroid function in rats is mediated by increased total and free thyroxine clearances concomitantly to increased activity of hepatic enzymes. Toxicology. (2009) 255:38–44. doi: 10.1016/j.tox.2008.09.026
- Ferreira M, De Oliveira PR, Denardi SE, Bechara GH, MAthias MIC. Fipronil (active ingredient of acaricide frontline®) acting on the mice thyroid. Microsc Res Tech. (2012) 75:265–70. doi: 10.1002/jemt.21053
- Leghait J, Gayrard V, Picard-Hagen N, Camp M, Perdu E, Toutain PL, et al. Fipronil-induced disruption of thyroid function in rats is mediated by increased total and free thyroxine clearances concomitantly to increased activity of hepatic enzymes. Toxicology. (2009) 255:38–44. doi: 10.1016/j.tox.2008.09.026
- Roques BB, Lacroix MZ, Puel S, Gayrard V, Picard-Hagen N, Jouanin I, et al. CYP450-Dependent biotransformation of the insecticide fipronil into fipronil sulfone can mediate fipronil-induced thyroid disruption in rats. Toxicol Sci. (2012) 127:29–41. doi: 10.1093/toxsci/kfs094
- Moser VC, Stewart N, Freeborn DL, Crooks J, MacMillan DK, Hedge JM, et al. Assessment of serum biomarkers in rats after exposure to pesticides of different chemical classes. Toxicol Appl Pharmacol. (2015) 282:161–74. doi: 10.1016/j.taap.2014.11.016
- Roques B, Leghait J, Martin PGP, Pineau T, Viguie C. The nuclear receptors pregnane X receptor and constitutive androstane receptor contribute to the impact of fipronil on hepatic gene expression linked to thyroid hormone metabolism. Biochem Pharmacol. (2013) 86:997–1039. doi: 10.1016/j.bcp.2013.08.012
- Simon-Delso N, Amaral-Rogers V, Belzunces LP, Bonmatin JM, Chagnon M, Downs C, et al. Systemic insecticides (neonicotinoids and fipronil): trends, uses, mode of action and metabolites. Environ Sci Pollut Res. (2015) 22:5–34. doi: 10.1007/s11356-014-3470-y
- Minnema DJ, Li AA, Collier RH, Sheets LP, Peffer RC, Creek MR. A critical review of neonicotinoid insecticides for developmental neurotoxicity. Crit Rev Toxicol. (2015) 46:153–90. doi: 10.3109/10408444.2015.1090948
- Simn-Delso N, Amaral-Rogers V, Belzunces LP, Bonmatin JM, Chagnon M, Downs C, et al. Systemic insecticides (neonicotinoids and fipronil): trends, uses, mode of action and metabolites. Environ Sci Pollut Res. (2015) 22:5–34. doi: 10.1007/s11356-014-3470-yo
- Pollak P. Fine Chemicals. Hoboken, NJ: John Wiley and Sons, Inc. (2011).
- Minnema DJ, Li AA, Collier RH, Sheets LP, Peffer RC, Creek MR. A critical review of neonicotinoid insecticides for developmental neurotoxicity. Crit Rev Toxicol. (2015) 46:153–90. doi: 10.3109/10408444.2015.1090948
- Rose PH. Chapter 6. Nicotine and the neonicotinoids. Royal Society of Chemistry. p. 184–220. doi: 10.1039/9781849733007-00184
- Gunier RB, Bradman A, Harley KG, Kogut K, Eskenazi B. Prenatal residential proximity to agricultural pesticide use and IQ in 7-year-old children. Environ Heal Perspect. (2017) 125:057002. doi: 10.1289/EHP504
- Pandey SP, Mohanty B. The neonicotinoid pesticide imidacloprid and the dithiocarbamate fungicide mancozeb disrupt the pituitary-thyroid axis of a wildlife bird. Chemosphere. (2015) 122:227–34. doi: 10.1016/j.chemosphere.2014.11.061
- Zhang ZY, Yu XY, Wang DL, Yan HJ, Liu XJ. Acute toxicity to zebrafish of two organophosphates and four pyrethroids and their binary mixtures. Pest Manag Sci. (2010) 66:84–9. doi: 10.1002/ps.1834
- Kortenkamp A. Ten years of mixing cocktails: a review of combination effects of endocrine-disrupting chemicals. Environ Health Perspect. (2007) 115(Suppl. 1):98–105. doi: 10.1289/ehp.9357
- Vandenberg LN. Low-dose effects of hormones and endocrine disruptors. In: Vitamins and Hormones (Elsevier Inc.). p. 129–165. doi: 10.1016/B978-0-12-800095-3.00005-5lze M, Silva E, Kortenkamp A. Extending the applicability of the dose addition model to the assessment of chemical mixtures of partial agonists by using a novel toxic unit extrapolation method. PLoS ONE. (2014) 9:e88808. doi: 10.1371/journal.pone.0088808
- Scholze M, Silva E, Kortenkamp A. Extending the applicability of the dose addition model to the assessment of chemical mixtures of partial agonists by using a novel toxic unit extrapolation method. PLoS ONE. (2014) 9:e88808. doi: 10.1371/journal.pone.0088808
- Bornehag C, Gennings C. A novel approach to chemical mixture risk assessment – Linking data from population based epidemiology and experimental animal tests. Toxicol Lett. (2018) 295:S52. doi: 10.1016/j.toxlet.2018.06.1203
- Flippin JL, Hedge JM, DeVito MJ, Leblanc GA, Crofton KM. Predictive modeling of a mixture of thyroid hormone disrupting chemicals that affect production and clearance of thyroxine. Int J Toxicol. (2009) 28:368–81. doi: 10.1177/1091581809341883
- Wu S, Li X, Liu X, Yang G, An X, Wang Q, et al. Joint toxic effects of triazophos and imidacloprid on zebrafish (Danio rerio). Environ Pollut. (2018) 235:470–81. doi: 10.1016/j.envpol.2017.12.120
- Bhaskar R, Mohanty B. Pesticides in mixture disrupt metabolic regulation: In silico and in vivo analysis of cumulative toxicity of mancozeb and imidacloprid on body weight of mice. Gen Comp Endocrinol. (2014) 205:226–34. doi: 10.1016/j.ygcen.2014.02.007
- Du L, Li S, Qi L, Hou Y, Zeng Y, Xu W, et al. Metabonomic analysis of the joint toxic action of long-term low-level exposure to a mixture of four organophosphate pesticides in rat plasma. Mol Biosyst. (2014) 10:1153–1161. doi: 10.1039/C4MB00044G
- Pandey SP, Mohanty B. Disruption of the hypothalamic-pituitary-thyroid axis on co-exposures to dithiocarbamate and neonicotinoid pesticides: Study in a wildlife bird, Amandava amandava. Neurotoxicology. (2017) 60:16–22. doi: 10.1016/j.neuro.2017.02.010
- Pandey SP, Tsutsui K, Mohanty B. Endocrine disrupting pesticides impair the neuroendocrine regulation of reproductive behaviors and secondary sexual characters of red munia (Amandava amandava). Physiol Behav. (2017) 173:15–22. doi: 10.1016/j.physbeh.2017.01.030
- Landrigan PJ, Lambertini L, Birnbaum LS. A research strategy to discover the environmental causes of autism and neurodevelopmental disabilities. Environ Health Perspect. (2012) 120:2012–5. doi: 10.1289/ehp.1104285
- European Food Safety Authority (EFSA). Scientific Opinion on the identification of pesticides to be included in cumulative assessment groups on the basis of their toxicological profile. EFSA J. (2013) 11:3293. doi: 10.2903/sp.efsa.2014.EN-538
- Howdeshell KL. A model of the development of the brain as a construct of the thyroid system developing a timeline model of thyroid system and brain. Environ Health Perspect. (2002) 110:337–348. doi: 10.1289/ehp.02110s3337
- Chapman TJ, Hillman SE, Boul LA, Kassotis CD, Dell CO, Robert J, et al. Developmental exposure to a mixture of 23 chemicals associated with unconventional oil and gas operations alters the immune system of mice. Toxicol Sci. (2018) 163:639–54. doi: 10.1093/toxsci/kfy066.
- Robert J, Mcguire CC, Kim F, Nagel SC, Price SJ, Lawrence P, et al. Water contaminants associated with unconventional oil and gas extraction cause immunotoxicity to amphibian tadpoles. Toxicol Sci. (2018) 166:39–50. doi: 10.1093/toxsci/kfy179
- Grandjean P, Andersen EW. Serum vaccine antibody concentrations in children exposed to perfluorinated compounds. JAMA. (2012) 307:391–7. doi: 10.1001/jama.2011.2034
- Milner BAM, Boyd IL. Toward pesticidovigilance. Science. (2017) 357:1232–4. doi: 10.1126/science.aan2683
- Andersson N, Arena M, Auteri D, Barmaz S, Grignard E, Kienzler A, et al. Guidance for the identification of endocrine disruptors in the context of Regulations (EU) No 528/2012 and (EC) No 1107/2009. EFSA J. (2018) 16:1–135. doi: 10.2903/j.efsa.2018.5311
- Andersson N, Arena M, Auteri D, Barmaz S, Grignard E, Kienzler A, et al. Guidance for the identification of endocrine disruptors in the context of Regulations (EU) No 528/2012 and (EC) No 1107/2009. EFSA J. (2018) 16:1–135. doi: 10.2903/j.efsa.2018.5311
- EFSA. Guidance on biological relevance. Draft version for public consultation. EFSA J. (2019) 1–60.